Substance Use - Data
Consultations
Drug and alcohol problems can contribute to both health and social harm and has both short- and long-term impact. Some of these problems are primarily social in nature, involving, for example, increases in acquisitive crime, prostitution, unemployment, family breakdown and homelessness (ScotPHO, 2023). Others are more clearly associated with health problems, for example, the transmission of communicable diseases (HIV, hepatitis), injecting-related injuries, longer-term irreversible illnesses, and death such as a range of cancers, fertility problems, nervous system issues, liver disease and cirrhosis (ScotPHO, 2023)
All can increase demands upon health and social care services.
Drugs
Problem drug use is defined as the ‘problematic use of opiates (including illicit and prescribed methadone use) and/or the illicit use of benzodiazepines and implies routine and prolonged use as opposed to recreational and occasional drug use’. A consequence of this definition is that people who use stimulants such as cocaine and amphetamines are not recorded in local and national figures.
Due to the illicit nature of drugs misuse, it is difficult to say how many people have problems with drugs. Data is collected for people attending a treatment service usually for addiction to an opiate (e.g., heroin) and/or benzodiazepine (e.g., Valium).
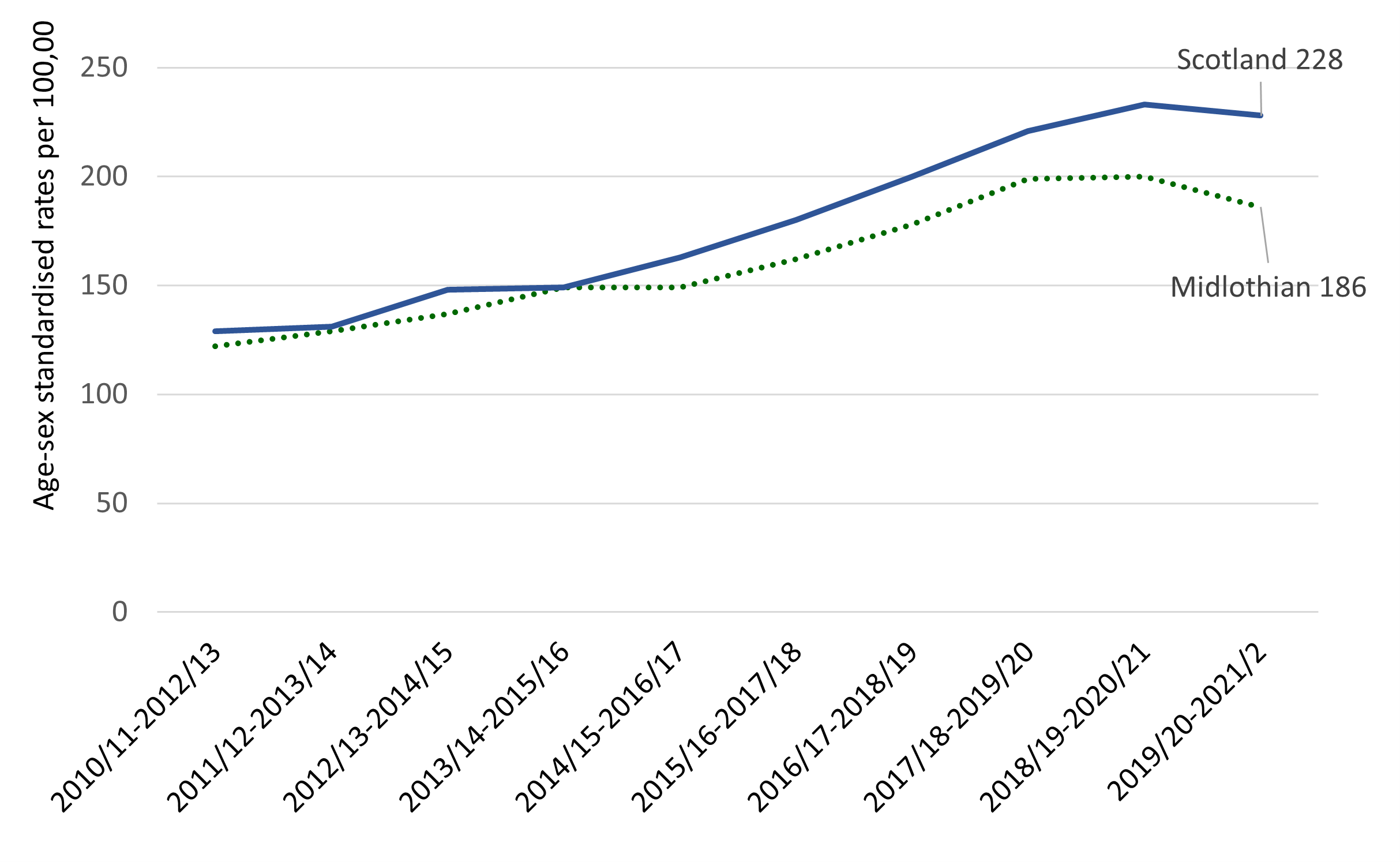
Drug-related hospital stays, 3-year aggregates, Midlothian and Scotland
Data Source: Scottish Public Health Observatory
Drug related deaths in Midlothian (1996 – 2022)
Data Source: National Records of Scotland
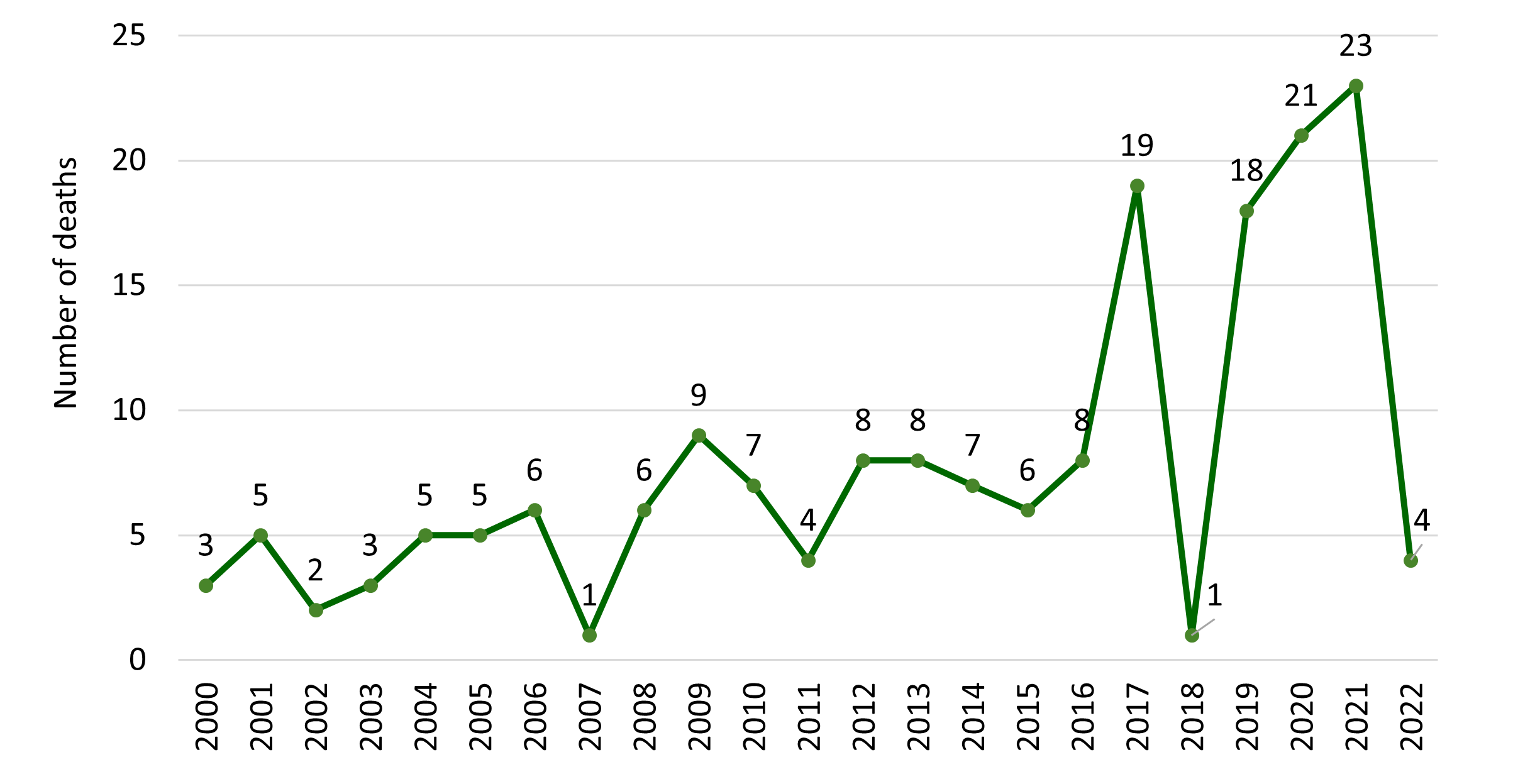
The five-year average drug related deaths in Midlothian were
- 3 for 1998-2002
- 4 for 2003-2007
- 7 for 2008-2012
- 6 for 2013-2017
- 16 for 2018-2022
Alcohol Related Harm
Alcohol can also lead to mental health problems, for example, alcohol dependency and increased risk of suicide. It is also linked to social harms such as traffic offences and accidents, anti-social behaviour, child neglect, violence against women and girls, family disruption, absenteeism from work and financial difficulties.
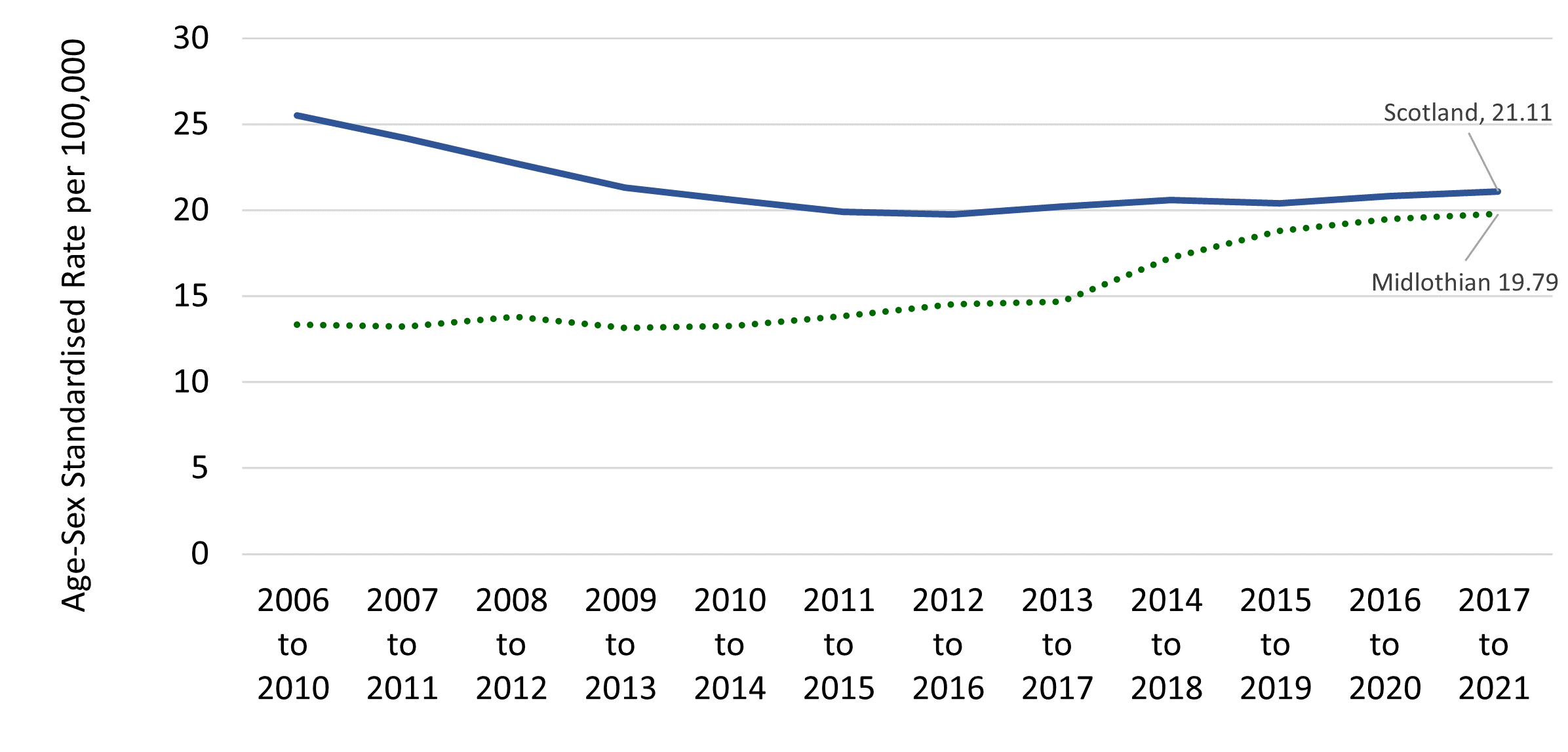
Alcohol specific deaths: 18 alcohol related deaths (2020) with a five-year average of 18 (2016-2020). The average age-standardised death rate for the five-year aggregate 2018-2022 was 18.2 deaths per 100,000 population, which is lower than the average Scotland rate of 23.4 over the same period.
Nationally statistics include conditions where each death is a direct consequence of alcohol misuse. They do not include deaths due to diseases for which alcohol is a risk factor (such as cancer). However, studies suggest that the number of deaths where alcohol was a contributory or risk factor is much larger.
Deaths from Alcohol conditions (rolling 5 year average)
Data Source: Scottish Public Health Observatory
Alcohol related hospital stays are the number of general acute inpatient and day case stays with a diagnosis of alcohol misuse in any position: 412 patients in Midlothian had alcohol related hospital admissions (2021/2022).
General acute inpatient and day case stays with an alcohol-related diagnosis in any position
Data Source: Scottish Public Health Observatory
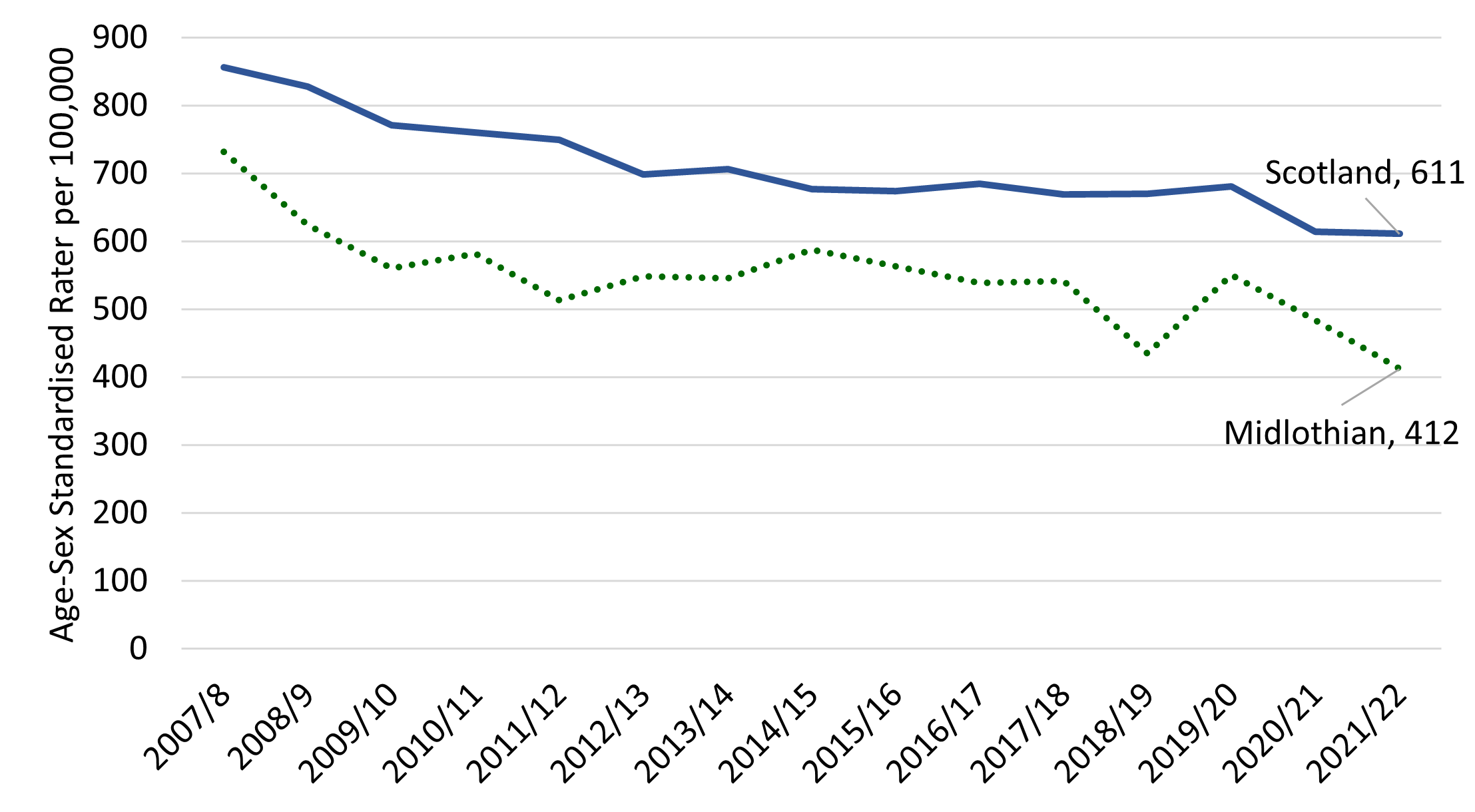
Fourteen of Midlothian’s intermediate zones sit above the Midlothian average for alcohol related hospital stays including (rate of admissions per 100,000 population):
- Dalkeith (1,059)
- North Gorebridge (746)
- Straiton (665)
- Penicuik Southwest (644)
- Easthouses (600)
- Bonnyrigg North (583)
- Penicuik Southeast (555)
- Thornybank (555)
- Mayfield (505
- Rural South Midlothian (483)
- Roslin & Bilston (466)
- Loanhead (466)
- Gorebridge & Middleton (534)
- Pentland (41)
While the data for Midlothian is better than the national picture there are challenges in tackling alcohol consumption. Alcohol related deaths in Midlothian have been increasing over the last decade. It is reasonable to assume based on national data that alcohol related harm is most acutely felt in Midlothian’s most deprived communities. Availability, affordability and consumption are key areas to help reduce alcohol problems. Audit Scotland reported a lack of evidence of the impact that services were having on their local communities and stigma remained a significant barrier to treatment and support.
Page updated: June 2024
